- 15 mass casualty incidents from regime airstrikes reported in Arakan State since 2023
- Kyaukphyu IDPs forced to flee again amid junta airstrikes and artillery attacks
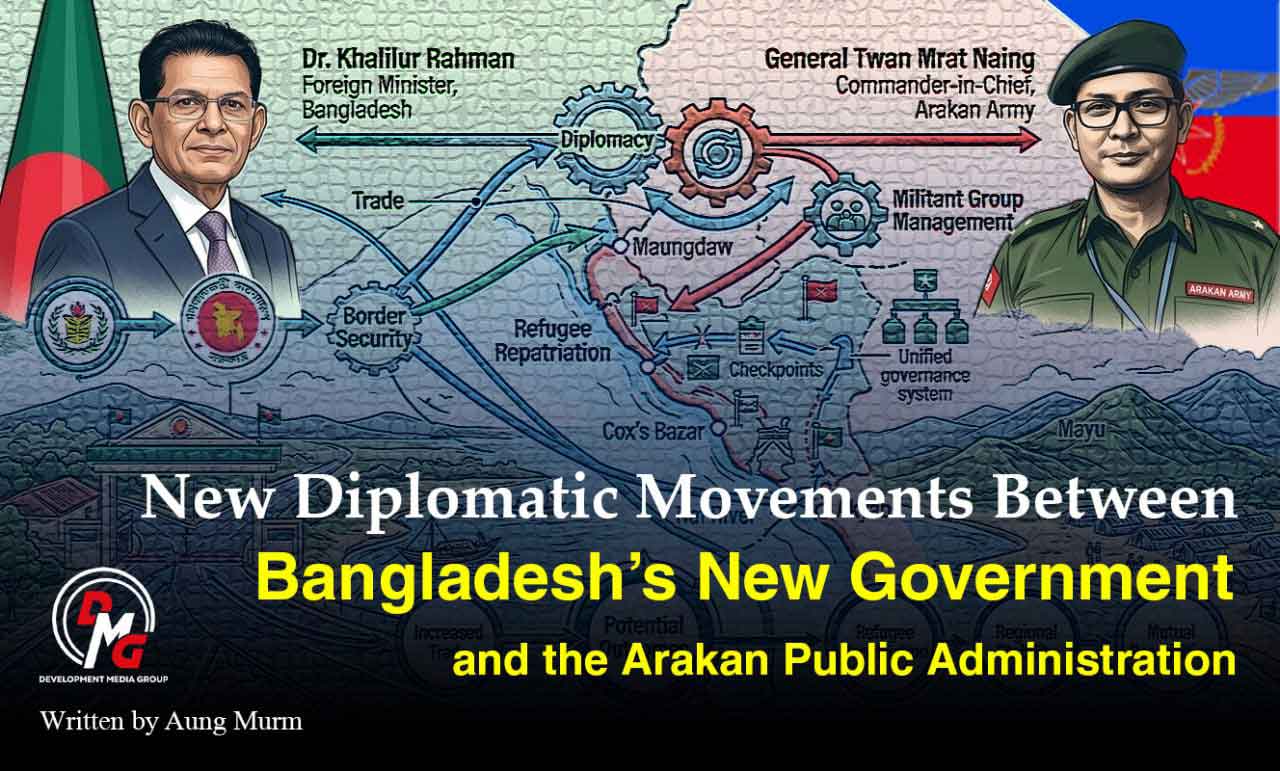
- New Diplomatic Movements Between Bangladesh’s New Government and the Arakan Public Administration
- Junta claims over 24 million ballots cast in 2025 poll, cites strong youth turnout
- ULA expands HIV prevention, healthcare services for sex workers in AA-held areas
Maternal Mortality and the Nation's Future
Maternal death devastates families and society: it constrains the lifelong development of surviving children and brings profound social and economic losses to households, communities, and the nation.
22 Oct 2025
Written By Ohn Taw
There are differing interpretations when defining maternal mortality. The World Health Organization (WHO) defines a maternal death as the death of a woman during pregnancy or within 42 days of termination of pregnancy, from causes related to or aggravated by the pregnancy or its management. The U.S. Centers for Disease Control and Prevention (CDC), meanwhile, tracks pregnancy-associated deaths occurring within one year of pregnancy.
The American College of Obstetricians and Gynecologists (ACOG) also uses a broad lens, counting all deaths during pregnancy and within one year postpartum, including both direct pregnancy-related and indirect causes. In short: WHO uses a 42-day postpartum window; CDC/ACOG often extend surveillance to one year postpartum.
Why do maternal deaths occur?
Maternal deaths arise from both direct obstetric and indirect causes. About 75% are directly linked to complications during pregnancy, childbirth, and the postpartum period. According to a The Lancet analysis covering 1990-2013, leading global causes include postpartum hemorrhage (15%), complications of abortion (15%), hypertensive disorders of pregnancy (10%), postpartum/puerperal infections (8%), and labor/obstructed delivery complications (6%). Pre-existing conditions-such as malnutrition and cardiac disease-account for up to 28% of maternal deaths.
Indirect contributors include maternal age, obesity, chronic illnesses, malaria, anemia, HIV/AIDS, and cardiovascular disease. Unintentional injuries (e.g., road traffic crashes, firearm/explosive injuries) also pose serious risks.
The "Three Delays" model
Beyond medical factors, systemic and social determinants drive maternal deaths, captured in the Three Delays Model:
1. Delay in deciding to seek care; 2. Delay in reaching a health facility; 3. Delay in receiving adequate, appropriate care at the facility.
Decision delays reflect family influence over women's health choices, poor awareness of danger signs, limited autonomy (e.g., inability to overrule in-laws), reliance on traditional beliefs ("home birth is fine"), and financial constraints.
Access delays stem from long distances, poor roads/transport, and low trust in services. Care delays include stock-outs (antibiotics, blood), shortages of skilled staff (physicians, midwives, nurses), misdiagnosis, negligence/poor quality, and unaffordable costs. These delays intertwine with socioeconomic status and culture, creating a complex web of risk.
Current situation
Up-to-date, comprehensive data for Arakan State are hard to obtain. According to the 2014 census, Myanmar's maternal mortality ratio (MMR) was 281.6 per 100,000 live births, and Arakan's was 314.3.
In high-income countries today, leading causes tend to be cardiovascular and mental health-related, whereas in low- and middle-income countries, the classic direct causes and the Three Delays still dominate. WHO's 2023 brief notes that every two minutes a woman dies from pregnancy-related causes. Average MMRs are about 346 per 100,000 in developing countries versus 10 per 100,000 in developed countries.
During COVID-19, maternal mortality worsened: globally, MMR rose from 211 (2020) to 242 (2021) per 100,000 live births. Given Arakan's realities-conflicts in 2019-20, the 2021-22 COVID period, renewed fighting in 2023, and intense conflict through 2024-25-many maternal deaths have likely gone unrecorded.
The path to prevention
UNFPA highlights four core actions:
1. Ensure quality antenatal care-at least four visits-with continuous monitoring of mother and fetus; 2. Ensure skilled attendance at birth (doctors, nurses, midwives); 3. Provide emergency obstetric and newborn care for complications; 4. Ensure postpartum continuity of care through 42 days (six weeks) after delivery.
Women also need trusted, accurate information on miscarriage and abortion. Where abortion is legal and safe, access to safe services significantly reduces deaths associated with unsafe abortion.
Maternal Death Surveillance and Response (MDSR) systematically identifies, reviews, and learns from each maternal death to prevent similar tragedies. WHO introduced MDSR guidance in 2013; by 2023, WHO reported that over 60% of maternal deaths are preventable.
A public-health perspective
Evidence shows a public-health approach-root-cause analysis plus practical interventions-is the most effective way to reduce maternal deaths. Maternal death review committees examine each case to recommend prevention strategies. Expanding sexual and reproductive health services reduces unintended pregnancies; comprehensive sexuality education helps prevent STIs and adolescent pregnancies.
Access is pivotal: cost, facility location, skilled providers, and reasonable travel distance underpin good outcomes. Where skilled staff are available in accessible facilities, MMR falls. Health-literacy programs that strengthen community decision-making and trust between patients and the health system benefit all-especially pregnant women.
Policy dimension
Maternal health entered the global agenda via the Millennium Development Goals (MDGs) and, in 2012, the Sustainable Development Goals (SDGs) through 2030. SDG 3 targets reducing global MMR to fewer than 70 per 100,000 live births and raising skilled birth attendance to 80%+.
Progress depends on political commitment. A study comparing Rwanda, Malawi, Niger, and Uganda found Rwanda's gains anchored in:
1. Reviewing and localizing policy into practice; 2. Promoting standardized provider guidelines; 3. Advancing context-specific solutions suited to local realities.
Why maternal mortality matters
Maternal death devastates families and society: it constrains the lifelong development of surviving children and brings profound social and economic losses to households, communities, and the nation. The loss of a mother's caring hands often steers families toward hardship. MMR is a barometer of population health-and a lens on the strength of the health system and stability of governance.
Breaking the cycle requires multi-sector action beyond health-transport, the economy, nutrition, and consistent access to safe, adequate food.
May many helping hands come together to secure maternal health and well-being.




.jpg)